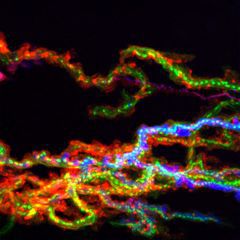
The inflammatory response serves a dual function. On the one hand, it deploys robust circuits of humoral and cell-mediated effector mechanisms to protect the host from harmful pathogens, both directly, through innate, rapid-onset processes and indirectly, by eliciting the adaptive arm of the immune response. On the other hand, the inflammatory response has co-evolved complex and partially overlapping mechanisms that contribute to tissue healing and regeneration (1). Ill-defined subpopulations of inflammatory cells sharing common lineage origin, for example monocytes and macrophages, acquire effector phenotypes that either sustain the inflammatory response or contribute to the healing process, through neo-vascularization and re-epithelization of injured tissues (2, 3). The environmental cues and signaling pathways underlying the aforementioned functional specialization of inflammatory cells are incompletely defined. The availability of more selective anti-inflammatory drugs would be beneficial in high morbidity disorders ranging from chronic inflammatory diseases, in which deregulated or persistent tissue infiltration by inflammatory cells contribute to tissue damage (4), to cancer, in which selected inflammatory cell subsets promote disease progression through the release of pro-angiogenic, ECM-remodeling or growth-stimulating factors (5). The inflammatory milieu exposes resident cells to a complex “bar code” of molecular cues and extracellular stimuli that require proper sensing and decoding. During leukocyte extravasation and interstitial migration, chemokines (CK) control a wide range of cellular functions that persist well beyond the rapid kinetics of G protein uncoupling and homologous desensitization of the membrane-expressed receptor. In recent years, Lefkowitz and coworkers (6) have shown that selected G protein-coupled receptors (GPCR) trigger a G protein-independent signaling cascade that involves a scaffolding function of receptor-associated beta arrestins (bARR).
The capacity of several chemokines to control transcriptional activity through modulation of MAPK signaling has already been clearly demonstrated (10, 11). The MAPKs can control events both in the nucleus, such as gene regulation, and in other compartments, such as cytoskeletal reorganization, through phosphorylation and activation of cytosolic targets (12). Several small-molecule inhibitors of p38 kinase have been generated and characterized, but their development was discontinued due to unacceptable safety profiles (13, 14).
The kinase MAPK Activated Protein Kinase 2 (MAPKAP2, or MK2), a downstream effector of p38 involved in TNF-α production, is a promising drug target for several inflammatory diseases (15). Our recent data have shown that MK2 is the main effector accounting for the ability of the SAPK pathway to stabilize selected mRNA carrying AU-rich elements (ARE) in their 3'UTR (16, 17). Our findings indicate that MK2 is synergistically activated by chemokines and adhesion receptors in several inflammatory cell types.
Altogether, these recent findings raise the intriguing possibility that signaling by chemokines at inflamed sites, besides directing cell migration, would be a required step to sensitize tissue-infiltrating leukocytes to multiple stimuli to be perceived as "dangerous" and to direct the activity of SAPK networks towards specific intracellular substrates.
- Medzhitov, R. Origins and physiological roles of inflammation (2008). Nature 454: 427-435.
- Mantovani A. et al. (2002). Trends Immunol. 23:549.
- Sonneman KJ and Bement WM. (2011). Annu. Rev. Cell Dev. Biol. 27:237-263.
- Nathan, C. and Ding. A. 2010. Cell 140:82011) Nucl Ac Res 39:2503.
- Qian, B and Pollard JW. 2010. Cell 141:210.
- Lefkowitz, R. et al. (2005). Transduction of receptor signals by beta arrestins. Science. 308:512.
- Smoler JS and Steiner G. (2003). Nat Rev Drug Discov. 2:473.
- Wells TN et al. (2006) Trends Pharmacol Sci. 27:42.
- Molteni R, et al. Blood 2009. 114:1073-1082.
- Kuwabara T. (2012). JLB 92:309.
- Gaestel M et al. (2009) Nat Rev drug Discov. 8:481.
- Fyhrquist N (2010) J. Invest. Dermatol. 130:342.
- Pettus RH and Wurz RP (2008) Curr Top. Med. Chem. 8:1452.
- Nebreda, A. R and Cohen, P. (2003) EMBO J. 22:5793.
- Gaestel M. (2006). Nat. Rev. Cell Biol. Mol. 7:121.
- Ramgolan, VS. et al. 2010. PLoS One 5:14450
- Zhang, J. et al. 2012. Am. J. Pathol.180:1751-1760